Understanding Risks of a Multiple Pregnancy
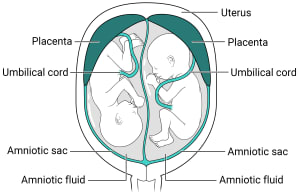
Twins with two placentas and two amniotic sacs.
Why is a multiple pregnancy a concern?
A multiple pregnancy means being pregnant with more than one baby. It is often a happy event for many couples. But multiple pregnancy has higher risks for complications. The most common problems are listed below.
Preterm labor and birth
More than 3 in 5 twins and nearly all higher-order multiples are preterm (born before 37 weeks). The higher the number of babies in the pregnancy, the greater the risk for early birth.
Preterm babies are born before their bodies and organ systems have fully matured. These babies are often small, with low birth weights. This means less than 5.5 pounds (2,500 grams). They may need help breathing, eating, fighting infection, and staying warm.
Very preterm babies are those born before 28 weeks. They are more at risk. Many of their organs may not be ready for life outside the mother's uterus and may be too immature to work well. Many multiple birth babies will need care in a neonatal intensive care unit (NICU).
Gestational high blood pressure
Women pregnant with multiple babies are more than twice as likely to develop high blood pressure of pregnancy. This health problem often starts earlier and is worse than in pregnancy with one baby. It can also raise the chance of early detachment of the placenta (placental abruption).
Gestational diabetes
Women with a multiple pregnancy are more likely to get gestational diabetes.
Anemia
Anemia is more than twice as common in women pregnant with more than one baby.
Birth defects
Multiple birth babies have about twice the risk for certain problems present at birth (congenital). These include spina bifida and other neural tube defects, and problems of the digestive tract and heart.
Miscarriage
A phenomenon called vanishing twin syndrome is more likely in multiple pregnancies. It's when more than one fetus is found, but vanishes (or is miscarried). This often happens in the first trimester. This may come with bleeding. The risk of pregnancy loss is higher in later trimesters as well.
Twin-to-twin transfusion syndrome
Twin-to-twin transfusion syndrome (TTTS) is a condition of the placenta that develops only with identical twins that share a placenta. Blood vessels connect within the placenta and divert blood from one baby to the other. It happens in about 3 in 20 twins with a shared placenta.
In TTTS, blood is shunted from one baby to the other through blood vessel connections in a shared placenta. Over time, the recipient baby gets too much blood. This can overload the cardiovascular system and cause too much amniotic fluid to develop. The smaller donor baby does not get enough blood and has low amounts of amniotic fluid. TTTS can be treated during pregnancy by withdrawing some of the extra fluid with a needle or with surgery on the placenta. Sometimes, the twins may need to be delivered early.
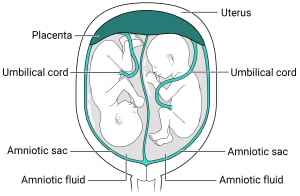
Twins with one placenta and two amniotic sacs.
Abnormal amounts of amniotic fluid
Amniotic fluid problems are more common in multiple pregnancies, especially for twins that share a placenta.
Cord entanglement
The umbilical cord for twins that share an amniotic sac can become tangled up. In these cases, the babies may need to be monitored often in the third trimester.
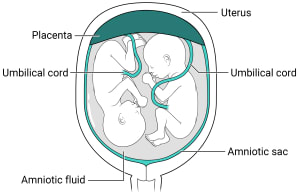
Twins with one placenta and one amniotic sac.
Cesarean (C-section) delivery
Abnormal positions of babies in the womb raise the chances of a C-section.
Postpartum hemorrhage
A larger placenta and larger uterus due to more babies place a mother at risk for bleeding after giving birth.